WARNING: Incredibly long post ahead, but since I haven’t made you read my ramblings in two months, we’re due for a glass of wine and a nice visit.
One of the most common things for me to hear these days is that I’m brave. I’m really not. And I’m not being falsely modest.
Bravery is an individual’s willingness to look death in the face, and then to take an action or actions that could bring death closer to that person, because the overriding need to achieve some other goal is more important.
(The argument could be made that just facing pain willingly would meet the definition of bravery, but I’m looking at the big picture concept here, and I think death—with its finality—is a better standard.)
Okay, so back to my level of brave. I don’t think I’m brave for choosing to be treated for a fatal disease. (And according to my husband, who refuses to be left raising a teen daughter alone, I had no choice!) I don’t believe I’m brave because I withstood multiple surgeries, chemotherapy and all that comes with those events. I won’t think I’m brave when I go into my next surgery, the DIEP flap reconstruction, which promises to be, from the upwards of two dozen-plus surgeries I’ve had in my adult lifetime, the most involved to perform and the most painful from which to recover.
Yes, there were many times during the last nine months when I was ready to just give it all up because my vulnerability, discomfort, and pain from surgery and treatments became too much. And we already know that my breaking point for chemo was the threat of losing my fingernails. (Which I still have, thank you very much.) That threat was strong enough for me to nix the very last of my 16 chemo sessions, with my doctor’s wholehearted approval, by the way.

These are my nails about three weeks after chemo ended. That white stuff? It’s the damage from the chemo, but it’s growing out and I didn’t lose any.
My ability to just look at the next step in front of me and get through it is based on a philosophy of not having any choice in the matter, because to me, I did not have a choice. I did not have a choice about cutting off my boobs—and the disease contained therein. I did not have a choice about losing my hair or enduring chemotherapy. I do not have a choice about my upcoming surgery. Cancer stripped me of choice and left me instead with “next steps.” My medical professionals, loved ones and God gifted me with the choice of life.
Hence, no bravery.
I’m a little more than seven weeks from my last chemo and I have finally found my brave.
I’ve reclaimed my body.
One of the very first thoughts I had on the afternoon of Aug. 5, 2016, when I learned that I had breast cancer, was that the next year of my life would now be dedicated to getting rid of cancer. I was absolutely correct. By the time I’m done with my reconstruction and recovery, it will be a little more than a year.

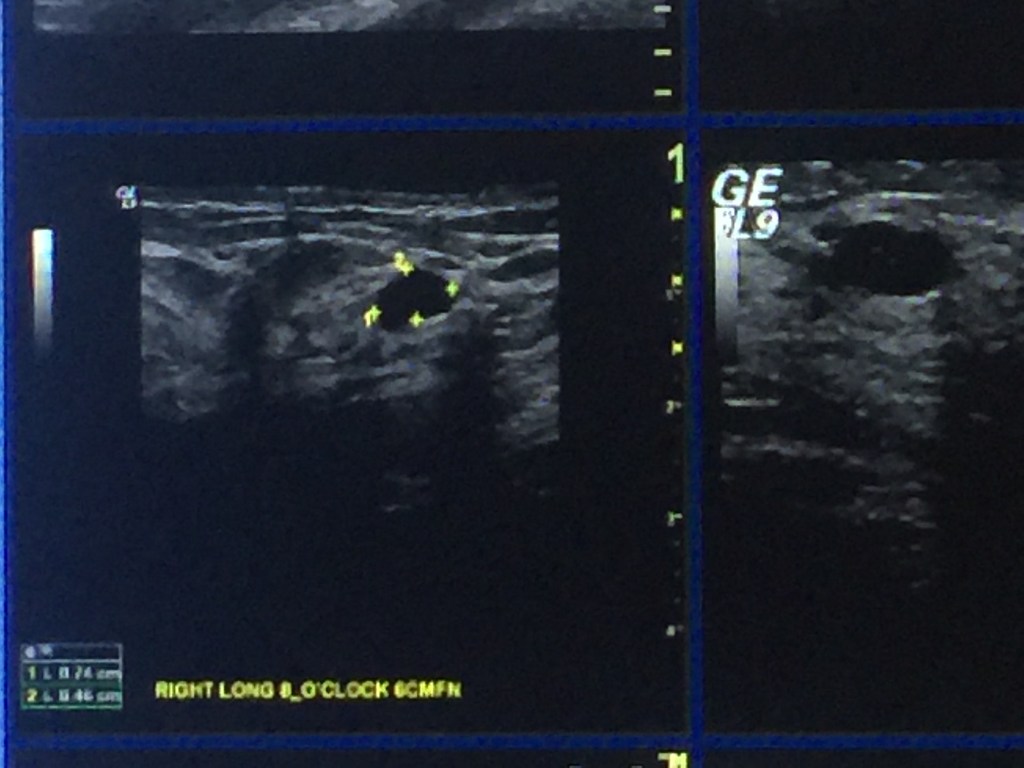
The initial breast ultrasound on July 25 that shows the first tumor found.
I’m happy to say that my life did not stop while going through treatments. I wouldn’t let it. To me, a year is way too long to give up on all of the wonderful moments that we’re entitled to experience. In this I did have a choice. I attended Sam’s functions as much as I physically could, and about the only reason I didn’t was if I had a conflicting appointment or if it was outside and too hot. (I don’t tolerate heat well and that fact has exacerbated with cancer treatments.) I maintained my membership in my groups and clubs, though sometimes attendance was spotty. I kept working, because I love my job and I like to think that I serve a purpose that’s not easily filled by others; at least I hope that’s the case. I visited with friends; attended holiday parties, special events and concerts; and even managed to survive one short business trip, complete with air travel and the TSA. All while having four surgeries, followed by bi-weekly and then weekly chemotherapy over an eight-month period. I am proud of myself for continuing to experience those things that bring joy to me and which define my life best: family, friends, fun activities and purposeful work. Yes, there have been many things I’ve had to say no to, or set aside for later days. But mostly I tried to maintain normal. I’m grateful that I was never too sick for too long to do all of this, as so many of my cancer friends are. In that I’ve been very lucky.

Sam and me at the Martina McBride concert about a week after my double mastectomy. I used a wheelchair and kept hoping Martina would call us out for being pathetically adorable, but the handicapped section of the theater was too far for her to see us. It’s OK Martina. We’ll catch you next time.
What I could not do was control my own body during this time. Every day, my bodily functions and the physical actions I took were dictated by cancer and the medical treatments needed to eradicate it from my body. The foods I ate, and when. The beverages I drank. The exercise, or lack thereof. The types of cosmetics I used and the supplements I took. The amazing and frightening amount of prescription medications available to me. The shots and the IVs and the tests that I had to survive. The clothes I wore. My hair—wanted and unwanted—nails and skin. All of these were controlled completely by cancer.
Cancer is a Body Snatcher.
At the end of my chemotherapy, I was 25 pounds heavier from what I weighed when I had my mastectomy in September. That’s on top of the 25 pounds I needed to lose before my cancer diagnosis. I had been working to that goal last year when I was diagnosed. I had rejoined a gym and was working out several times a week with a trainer to get in shape. I was about three months into this when I had that fateful mammogram that revealed my cancer. I couldn’t work out while I was going through and recovering from surgery and then, when I started chemotherapy about four weeks later, I couldn’t get anywhere near the gym because it is the best germ factory known to mankind, (outside of the secret storage labs in the CDC, that is). My gym put my membership on hold and I tried to keep up some movement at home, but too many days and nights I was just too tired to move, especially if I was working that day. Honestly, it was all I could do most days to just get up and dress for work, because my energy was so sapped from treatment.
The first month after finishing chemo, I gave my body the time it needed to come back to normal. It’s mostly there. The main side effects I had with the three different chemo drugs I was on were heartburn; hot flashes; exhaustion; neuropathy (nerve damage in hands and feet—painful at best, numb at worst); hair loss; bloating; low-grade nausea; diarrhea; muscle aches; and here’s the worst: the thinning of my body’s membranes, which caused my nose to constantly bleed, me to never get a full night’s sleep, and other nasty related issues.

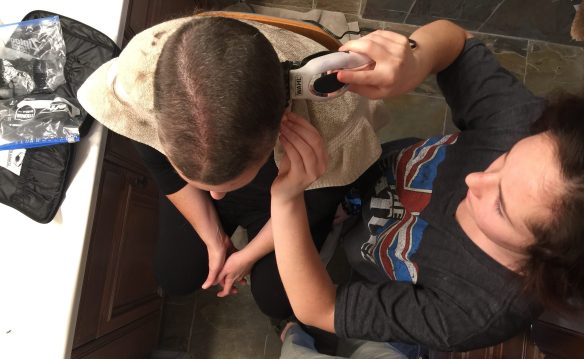
Stephen lovingly calls the top of my head the “landing strip.” Because I lost this section of hair last (think short mohawk people), it’s the last to come back.
(The only good side effect from chemo was that my skin never looked better. A dermatologist told that he’s seen this before, that the chemo kills all toxins, including the stuff that makes our skin gross. So, yay for that at least!)
I’m thrilled to share that most of these issues are gone or resolved. I have Baby Chick Fuzz growing on my head, I’m shaving my underarms again (yep, you heard it here first, folks), I have most of my energy back, I haven’t taken heartburn meds in two weeks, and my nose—my poor, poor nose—is no longer bleeding. Hot flashes apparently will always be with me now and the neuropathy in my feet is still a factor. But the rest is gone.
Three weeks ago, I reactivated my gym membership. (They were awesome working with me at Crunch. Flexible and kind, they froze my account with no hassle and stashed my “banked” training hours until I could use them again. Thank you Crunch!!) I’ve been going three times a week since, using the bike and treadmill to slowly increase my stamina. Today I had my first appointment with my new trainer. C. has faced medical hurdles herself and was recommended to me for that. She is sweet and encouraging and right now I need someone like her to help me be kind to my body and bring me back to health.
So, about my brave…
I used to have a good body. I’m not being conceited, just factual. In my teens, 20s and early 30s, I rocked a size 4 in a near-perfect hourglass. Just ask Steve. He’ll tell you. I recovered from Samantha’s birth with a few extra pounds on me, but somewhere around that tragic age of 40 (tragic to a woman’s body, not to my life), the pounds started packing on. In my mid-40s I’d had enough and started working with an amazing trainer. For two years, we whipped me into shape. Then I lost my job, my brother was nearly killed in an accident and I had to take care of him, and my beloved trainer moved out of the area. The pounds packed on again.
But I was still not anywhere near as bad a year ago as what I’m face in the mirror today. The following is NOT written to elicit a) sympathy, b) disdain, or c) contradicting feedback. I’m sharing this to mark where my brave comes in. My body looks like I barely survived a landmine explosion. Of course, I’m boobless, until we get to next month’s surgery. All of the weight I’ve gained from the steroids during chemo has landed on my upper abdomen, my chest is a global map of surgery scars. I have extra skin that was intentionally pulled and tucked into my underarm area that is being “saved” for the reconstruction surgery. I look round on my belly and concave on my top. The only part of me that looks remotely normal are my legs. The added weight prevents me from wearing 90 percent of my fabulous wardrobe. I can only fit into loose, stretchy things right now. I can’t wear normal bras, even with my prosthetic boobs, because of the extra skin. (I tried for a week and because all of my nerves were cut during the mastectomy, I can’t feel pain my chest and didn’t see or realize that my bra had cut into my flesh, big time. Not good.)
We gain a lot of confidence and self-comfort from looking and feeling good. Speaking from the XX end of the chromosomes, most women spend many years and many dollars trying to achieve the most real and best version of ourselves that’s possible. It’s why I have to chuckle when my teen daughter moves into her bathroom for HOURS Every. Single. Night. I keep explaining to my hubby that she’s just trying to find the best version of herself so she can then move on to be brilliant in everything else she does.
Going to my gym regularly means that I am stripping, showering and dressing in front of mostly fit, sometimes incredibly fit, women of all ages. I’m waiting for the day when someone walks in and catches my round, boobless shape with my almost-bald head and thinks I’m a guy invading the women’s locker room. Or when some young thing stumbles into the vision of my scarred, messed-up chest and runs in horror from the sight. What I feel like most of the time is a freak, A female Quasimodo, who society will scorn because of my horrific body. I am absolutely not at my real and best version of myself these days.
Again, there’s no need to step in here and list out what I already know: that I’ve been through physical and emotional hell and have come out of it thriving; that my family and friends love me as I am; that I will get my body and life back together; that I’m not responsible for most of what’s happening here; and on.
What’s even more important to know that I know is that feelings are only my reality if I make them true. Most of the time I acknowledge the feeling of Freak-Hood and move on. But I still feel it. And when I’m at the gym, in these first few weeks, and am completely exposed and vulnerable, I just live through the experience as one big freak. It scares me, which is why I know I’ve found my brave.
I’m taking small but steady steps to make amends with my temporary Freak-Hood. I’m mostly not wearing my head coverings, because my fuzz is coming back and because it’s too damn hot most of the time. I’m sweating more than I have in years, voluntarily. I’m being kind to myself. Really, I am. I avoid pictures because I don’t need to be reminded in a year or five about how I feel right now. I take care with the rest of my appearance and I’m really rocking the eyebrows and good skin these days. I’ve tucked away my skinny clothes so they aren’t torturing me, but I expect to be wearing them in a couple of months. I also expect to be strong, and able to withstand this upcoming surgery as best as possible. (I talked about this surgery HERE if you’re curious about what it is.)

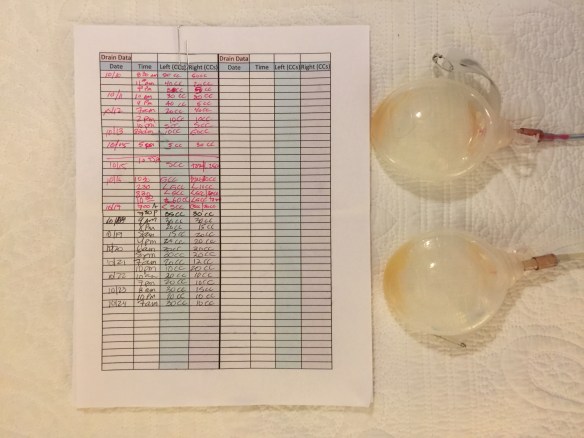
This is me taking my body back. As I have so many times before, I thank all of my body guardians (doctors, nurses, techs, family and friends—they all have a role in this) for the year of service they’ve given to me, and the ongoing maintenance. I really did have to just give my body to them, over and over again. It’s like I was battling my cancer, but so were they, my personal Army of Cancer Conquerors. So many times along this path, I’ve had to provide information and give up control in ways I’ve never imagined. Pretty hard for this Type A Introvert to do, but I did, because I knew that these people were my best chance to survive breast cancer.

Now it’s time to for me to take back some of the work and make myself strong and ready for the upcoming surgery (I have to come up with some catchy name for this surgery—suggestions are welcome) and beyond. I will move past Freak-Hood and into Fab-Hood, because that’s what we do when we’re done surviving and move into thriving. And I will do it bravely.